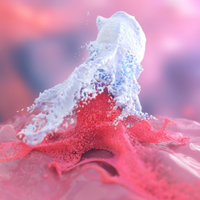
ABOVE: Illustration of macrophage a engulfing a cancer cell
© ISTOCK, MARCIN KLAPCZYNSKI
More than a century ago, Otto Aichel, a German pathologist, made the peculiar observation of cancer cells with characteristics of different cell types, including white blood cells. The data led him to propose that the fusion between cancer cells and white blood cells could impose advantages to the tumor, allowing it to spread more readily in the body. But since then, evidence for the formation of these cancer cell–immune cell hybrids has been difficult to come by.
Now, Aichel’s theory just got a lot more support. In a study published yesterday (September 12) in Science Advances, researchers at the Oregon Health & Science University (OSHU) and their colleagues describe the presence of such hybrids in mouse models of cancer and in the peripheral blood of patients with solid tumors.
In the human cancer patients, the...
“This is an excellent study with a solid study design and appropriate controls, particularly as cell fusion is a notoriously difficult cellular process to study,” Brenda Ogle, who studies cell-cell fusion at the University of Minnesota’s Stem Cell Institute and who was not involved in the work, writes in an email to The Scientist. “The authors’ results expand on prior work [in mice] to the clinic and make a compelling case for tracking circulating hybrid cells as a means to predict stage and survival outcomes in cancer patients.”
We found that these circulating tumor cell hybrids are an order of magnitude greater in number compared to standard circulating tumor cells and correlate with aggressive disease and patient outcomes.
—Melissa Wong, Oregon Health & Science University
OSHU’s Melissa Wong and her colleagues had previously demonstrated that culturing mouse colon cancer cells together with macrophages can result in cell hybrids with chromosomes from each cell type. They also provided hints that this process occurs in vivo.
In the new work, the team first validated that co-culturing mouse colon or melanoma cancer cell lines with macrophages resulted in a population of spontaneously fused hybrid cells. The researchers identified hybrid cells by looking for the simultaneous presence of recipient and donor fluorescent markers and sex chromosomes from both cell types present in the hybrid cells. They also captured the fusion process using live imaging and showed that the hybrids went on to divide.
The hybrid cells had a greater ability to migrate and invade in vitro compared to the unfused cancer cells, and when injected into mice, they more readily formed metastases compared to their nonhybrid cancer cell line counterparts. The researchers also observed spontaneous hybrid cells in mice injected with melanoma cells.

“The researchers conducted rigorous experiments to show the presence of the cell hybrids, the most important of which was the demonstration that these cell fusion hybrids acquire characteristics different from unfused cancer cells, including enhanced motility,” says John Pawelek of the Yale School of Medicine who also studies cell fusion in the context of cancer and was not involved in the study.
To understand whether hybrid cancer cells are also present in human cancer, Wong and her colleagues took advantage of a specific cancer scenario—a secondary solid tumor that arose in female cancer patients who had received a bone marrow transplant from male donors. These secondary cancers allowed the researchers to identify potential cell hybrids that contained a Y chromosome from the transplant. Tumor samples from seven women in the study all had solid tumor cells with a Y chromosome, indicative of cell fusion.
The team decided to see if they could detect such hybrid cells in blood samples from the patients—following their secondary cancer diagnosis—and found that in each case, the blood contained a population of cells that had both a solid tumor cell-surface marker and CD45, a blood cell marker. These circulating hybrid cells have not been identified previously in any study.
See “Cancer and Immune Cells Merge”
While circulating tumor cells (CTC) are generally rare in the blood of most cancer patients, the team found that circulating hybrid cells were more abundant than nonfused CTCs. The team then went on to show that these types of hybrid cells are also present in some pancreatic cancer patients and are also more abundant in their blood than normal CTCs.
The presence of the circulating hybrid cells appeared to be prognostic, correlating with a more advanced cancer stage of cancer and poorer survival. In contrast, CTCs did not help predict how the patients would fare.
“We found that these circulating tumor cell hybrids are an order of magnitude greater in number compared to standard circulating tumor cells and correlate with aggressive disease and patient outcomes,” says Wong. “This novel circulating tumor cell population has been previously overlooked.”
According to Ogle, the study builds on prior evidence of cancer fusions from animal studies that these hybrids “likely confer a high level of heterogeneity that might also be critical for tumor propagation.”
“These cancer hybrids are hard to detect in patients,” notes Pawelek. “We are currently dependent on patients who have received bone marrow transplants, but we need a new technique to test the hypothesis that cell fusion could be a mechanism of metastasis.”
Wong and her colleagues are now looking for these cancer cell hybrids in other tumor types and working to tease out the mechanism of cell fusion and identify ways to block this event.
C.E. Gast et al., “Cell fusion potentiates tumor heterogeneity and reveals circulating hybrid cells that correlate with stage and survival,” Science Advances, doi:10.1126/sciadv.aat7828, 2018.
Interested in reading more?