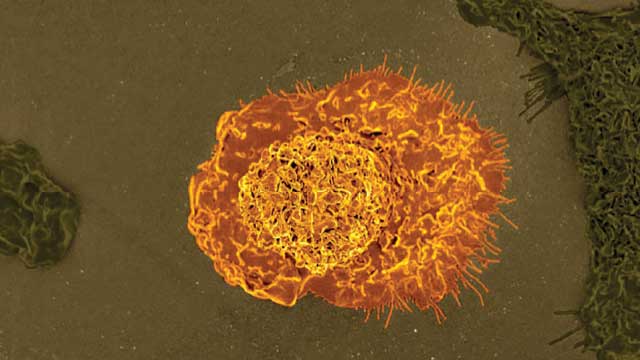
NOT ALL BAD: Macrophages, such as the one shown in this artificially colored scanning electron micrograph, may help or hinder cancer’s spread.D. PHILLIPS/SCIENCE PHOTO LIBRARYIn the late 2000s, Stanford University stem cell biologist Irving Weissman wanted to understand how normal blood-forming stem cells differed from those that went on to seed a type of blood cancer called acute myelogenous leukemia (AML). Using bone marrow samples from AML patients who had survived the nuclear bombs dropped on Japan during World War II, his team identified the developmental stage at which blood-forming stem cells branch off to become cancerous and compared gene expression profiles between those cells and their counterparts from healthy bone marrow samples. The researchers found that the leukemia-forming stem cells highly expressed a gene encoding CD47, a surface molecule known for its role on normal, healthy cells as a “don’t eat me” signal to phagocytosing macrophages....
NOT ALL BAD: Macrophages, such as the one shown in this artificially colored scanning electron micrograph, may help or hinder cancer’s spread.D. PHILLIPS/SCIENCE PHOTO LIBRARYIn the late 2000s, Stanford University stem cell biologist Irving Weissman wanted to understand how normal blood-forming stem cells differed from those that went on to seed a type of blood cancer called acute myelogenous leukemia (AML). Using bone marrow samples from AML patients who had survived the nuclear bombs dropped on Japan during World War II, his team identified the developmental stage at which blood-forming stem cells branch off to become cancerous and compared gene expression profiles between those cells and their counterparts from healthy bone marrow samples. The researchers found that the leukemia-forming stem cells highly expressed a gene encoding CD47, a surface molecule known for its role on normal, healthy cells as a “don’t eat me” signal to phagocytosing macrophages....
The researchers looked at stem cells from AML patients at the Stanford Medical Center to see if they also expressed CD47. “They all did,” says Weissman. After demonstrating in cell culture experiments that macrophages only engulfed AML cells that did not display CD47 on their surface, Weissman’s team grew human AML cells in five immune-deficient mice and treated the animals with an antibody against CD47.1 In just two weeks, AML cells were nearly undetectable in the animals’ blood, and had dropped by 60 percent in their bone marrow. “It was shocking,” says Weissman, noting that four of the five mice were essentially cured. “We knew that we were on the track of a potential therapeutic.”
In less than a decade, Weissman and his colleagues at Stanford have found CD47 on every type of cancer they’ve been able to get their hands on. Meanwhile, at least three biomedical companies, including the Stanford spin-off Forty Seven, Inc., have raised and invested tens of millions of dollars to test drugs that block the molecule. The approach seems so promising that last August, Rider and Victoria McDowell, inventors of the vitamin product Airborne, offered $10 million to anyone who would grant them access to an anti-CD47 therapeutic—none of which have yet been tested for pediatric use—to treat their 17-year-old son’s brain tumor.
I think now we are back to saying, “Maybe it’s just very complex.”—Mikael Pittet, Harvard Medical School
But back in 2008, when Weissman first tried to publish his work on how macrophages engulfed leukemia cells lacking CD47, his reviewers didn’t buy it. Since the 1980s, cancer researchers have linked macrophages and macrophage-stimulating genes to tumor growth and poor outcomes for cancer patients, and the cells had been pegged as nothing but bad news when it came to cancer. In 1996, for example, researchers from the University of Oxford reported that women whose breast cancer biopsies contained a high density of macrophages were much more likely to succumb to the disease over the subsequent five years than those with low densities.2 The same correlation was later confirmed in a dozen other types of cancer. These cells earned the name tumor-associated macrophages, or TAMs, and research focused on where they came from and how to block or deplete them. Weissman’s data suggesting that macrophages could help defeat cancer just didn’t fit.
“Several years ago, the idea was, ‘Let’s deplete these cells because they are bad,’” says Mikael Pittet, an immunologist at Harvard Medical School. Specifically, TAMs, which can make up as much as 50 percent of a tumor’s mass, had been found to repress other immune cell activity, encourage blood and lymph vessel development to support growing tumors, and help cancer cells metastasize to new sites in the body. But over the past decade, some research has surfaced to support Weissman’s conclusion that TAMs may have an upside, Pittet says. “I think now we are back to saying, ‘Maybe it’s just very complex.’”
Masters of metastasis
TAMs start out either as tissue-resident macrophages, which originate from the embryonic yolk sac and take on tissue-specific roles during development, or as monocytes, which are born in the bone marrow and circulate in blood until they are recruited to tissues throughout adulthood. Tumors secrete signaling molecules, such as colony-stimulating factor 1 (CSF-1) and CC chemokine ligand 2 (CCL2), that attract monocytes and tissue-resident macrophages and convert these cells to the cancer-supporting TAM phenotype.
In the mid-1990s, reports linking CSF-1 to cancer were rolling out one after the other, implicating macrophages as accomplices to tumors. But these studies didn’t explain how the immune cells influenced the course of a particular cancer. To make sense of this growing literature, Jeffrey Pollard, a developmental biologist at the University of Edinburgh in Scotland, worked with colleagues to create a mouse model prone to developing breast cancer that also lacked the gene encoding CSF-1. The model revealed that the absence of CSF-1 had no effect on whether primary breast cancer tumors grew, but it did reduce the density of TAMs in the tumors and delayed metastasis.3
It made sense to Pollard that the link between macrophages and survival would have to do with cancer’s spread. “The reason you die of cancer is metastasis,” he says. Pollard’s findings have since been repeated in several animal models of cancer, and CSF-1 signaling has become a popular target for developing cancer drugs. There are now more than a dozen ongoing clinical trials testing monoclonal antibodies and pharmacologic inhibitors that disrupt the pathway.
Pollard’s team has also found that TAMs help tumors metastasize by supporting tumor angiogenesis, or new blood vessel development.4 In addition to supplying conduits for oxygen, nutrients, and growth factors to support a tumor’s development, angiogenesis lays out a path for metastatic cells. Other researchers have homed in on a specific subgroup of TAMs responsible for this angiogenesis, identified by their production of the protein Tie2.5
Tie2-producing TAMs also appear to act as chaperones for traveling tumor cells. While recording cell movement inside breast cancer tumors in live mice, John Condeelis and his team at Albert Einstein College of Medicine in New York recently found that Tie2+ macrophages were always present as a cancer cell approached and entered a blood vessel. But the macrophages were doing more than just accompanying tumor cells. “When these macrophages and tumor cells started to approach the vasculature, they underwent this rather peculiar geometric transformation where they would form a pyramid-type structure on the vessel wall, and it had three cell types in it,” Condeelis explains.
The pyramid always contained a Tie2+ macrophage, a cancer cell overexpressing a protein called Mena, and a blood vessel endothelial cell, all three in contact with one another. This suite of cells, which the researchers called a tumor microenvironment of metastasis (TMEM), had to be present for tumors to metastasize.6 In the TMEM, Tie2+ TAMs make vascular endothelial growth factor (VEGF), which signals blood vessel endothelial cells to separate and allow cancer cells to slip into the bloodstream.7 In healthy tissues, Condeelis says, similar structures develop at sites where new blood vessel branches will bud. In breast cancer, “instead of generating a branch on the vessel, you generate a doorway on the vessel.”
Last year, the researchers reported that treating mice with breast or pancreatic tumors with an inhibitor of Tie2 called rebastinib kept Tie2+ macrophages out of the tumors, reduced the ability of cancer cells to enter nearby blood vessels, and improved the efficacy of two chemotherapy drugs.8 Condeelis has also licensed the use of TMEMs to the Boston-based company MetaStat, Inc. as a clinical cancer biomarker that predicts whether breast cancer patients will go on to develop a recurrence with metastatic tumors.9
TAMs also appear to play a role at sites on the receiving end of tumor metastasis. A population of macrophages distinguished by their expression of the VEGF receptor Flt1 are more likely to be found at sites of metastasis than in primary tumors, Pollard’s team found. When cancer cells traveling in the blood attach to a blood vessel wall, these macrophages, dubbed metastasis-associated macrophages (MAMs), are already waiting on the other side. In a study published in 2009, Pollard and colleagues used fluorescence microscopy to track tumor cells injected into the blood vessels of mouse lung slices and watched as the cells made contact with MAMs across the vessel walls.10 When the team depleted MAMs, the number of tumor cells that got across the vessel wall into the tissue dropped by 50 percent.
Helping cancer cells in and out of blood vessels are just some of the steps in a complex cascade of several rate-limiting events required for successful metastases, says Pollard, but in recent years it’s become clear that “macrophages enhance those rates.”
Tumor protectors
TAMs don’t just help cancers spread; they can also help tumors survive attacks from the immune system, and from currently available treatments. For example, a group at the Oregon Health & Science University recently reported that TAMs secrete a cytokine called IL-10 that prevents dendritic cells from activating antitumor T-cell responses.11 In some cancers, TAMs also produce transforming growth factor beta (TGF-β), which promotes survival of a subset of anti-inflammatory regulatory T cells, further blunting antitumor T-cell attacks.
 TWO-FACED MACROPHAGESTumors use chemokine signals to draw monocytes and tissue-resident macrophages into the tumor microenvironment, where the cells become tumor-associated macrophages (TAMs). Once believed to be wholly supportive of cancerous growth, these cells also play important roles in protecting against disease.
TWO-FACED MACROPHAGESTumors use chemokine signals to draw monocytes and tissue-resident macrophages into the tumor microenvironment, where the cells become tumor-associated macrophages (TAMs). Once believed to be wholly supportive of cancerous growth, these cells also play important roles in protecting against disease.
See full infographic: WEB | PDF© SCOTT LEIGHTON
Damage caused by radiation and many types of chemotherapy can also stimulate an influx of new TAMs to tumors, where the cells release molecules that promote cancer survival. At least one molecule responsible for this protective effect, identified by cancer biologist Johanna Joyce and her team at the University of Lausanne in Switzerland in 2011, is a protein-chopping enzyme called cathepsin. The researchers reported that TAMs release cathepsin in response to chemotherapy drugs and that cathepsins reduced tumor cell death after treatment with the chemotherapy drug paclitaxel (Taxol). Last year, they found that as-yet unidentified TAM-secreted molecules interfere with the ability of paclitaxel to induce DNA damage and to block mitosis in cancer cells.12
TAMs may also thwart cancer immunotherapies. Recently, Harvard’s Pittet and his team caught TAMs in the act of sequestering an anti-PD-1 treatment, which is meant to bind and activate tumor-killing T cells.13 Using high-resolution imaging in live mice, Pittet’s team found that within an hour of treatment, TAMs used antibody-binding receptors to steal the drug from the surface of T cells. When the researchers treated mice with antibodies that block the receptors on the TAMs before anti-PD-1 treatment, the drug remained on T cells at least twice as long, and the animals’ tumors shrank more over 10 days of treatment.
With so many ways that TAMs protect tumors, it’s no wonder many groups have found that blocking or depleting the cells in cancer models can improve T-cell responses and enhance the effect of cancer immunotherapy. For example, Mountain View, California–based biopharmaceutical company ChemoCentryx has developed a compound called CCX872, which blocks a receptor called CCR2 that monocytes use to find their way into areas of chronic inflammation. At the meeting of the American Association for Cancer Research last year, the company reported that in mice with pancreatic cancer, CCX872 treatment not only kept monocytes out of tumors, it also enhanced the animals’ responses to anti-PD-1 therapy. The company’s CEO Tom Schall says ChemoCentryx is currently designing another study to test this combination in humans. (See “Make Me a Match” here.)
Drugs that target chemokine interactions have great potential for peeling away the immunosuppressive effects of TAMs and improving patient response rates to therapies that activate T cells, Schall says. “I think this is an idea whose time has come.”
The good TAMs
Even as therapies that block TAM activity or prevent macrophage recruitment to tumors reach clinical trials, many researchers are not ready to give up on what macrophages may have to offer in the fight against cancer. Weissman’s work on CD47 is a prime example of TAMs’ cancer-killing potential.
 DOUBLE AGENTS: TAMs with the M2 phenotype promote cancer progression, while M1 TAMs suppress it.NIAID/FLICKR
DOUBLE AGENTS: TAMs with the M2 phenotype promote cancer progression, while M1 TAMs suppress it.NIAID/FLICKR
Since his initial discoveries, Weissman has focused on macrophages’ innate drive to eat damaged and dying cells, and he’s found that many cancers display an “eat me” signal—a molecule called calreticulin, which marks the cells for phagocytosis.14 But even if a cancer cell has “eat me” written all over it, presentation of CD47 can save it by engaging an inhibitory macrophage receptor called signal regulatory protein alpha (SIRPα). SIRPα blocks the molecular pathway that macrophages use to rearrange their structure and wrap themselves around the cells targeted for destruction. Weissman’s team has published a suite of papers showing that masking the “don’t eat me” signal can set macrophages loose against tumors in mouse models of AML, non-Hodgkin lymphoma, pancreatic cancer, and small cell lung cancer, as well as three different types of pediatric brain tumors. Like Forty Seven, Inc., Alexo Therapeutics and Trillium Therapeutics are preparing for Phase 2 trials of CD47-binding antibodies and fusion proteins, either alone or in combination with other drugs, including several immunotherapies.
Weissman says SIRPα is not the only gatekeeper molecule for macrophage phagocytosis. His group recently reported that some TAMs from human and mouse colon tumors display PD-1, the surface protein targeted by anti-PD-1 therapies to boost T-cell responses, and that these cells are worse at phagocytosing tumor cells than TAMs that don’t display PD-1, suggesting that PD-1 may be a second TAM gatekeeper.15 Indeed, the team reported that knocking out the PD-1 ligand in colon tumors in mice increased the phagocytosis activity of TAMs.
In some cases, Weissman argues, macrophages may aid cancer immunotherapies. For example, antibodies against CD20, which are used as an immunotherapy for some lymphomas, bind cancer cells in vitro and act as a tag that signals macrophages to engulf them.16 And his team has found that anti-CD47 synergizes with immunotherapeutic antibodies against CD20, the breast cancer marker HER2, and the lung cancer marker epidermal growth factor receptor in mouse models of each cancer type.17
Pollard says there’s no question that macrophages can participate in antitumor responses, “it’s just that the tumors develop a way of polarizing or educating those macrophages to help [the tumors] rather than destroy them.”
Recruit and re-educate
Many researchers are now taking advantage of macrophages’ plasticity to re-educate the cells to work for the patient. One way to switch TAMs from what’s known as the M2 phenotype, which promotes cancer growth, to the immune-boosting M1 phenotype is to provide the cells with proinflammatory stimuli, such as interferons or ligands for Toll-like receptors. Alternatively, researchers can directly target molecular switch proteins responsible for driving M2 characteristics, such as PI3-kinase and the transcription factor STAT3. In animal models, drugs that inhibit these molecules have successfully skewed TAMs toward M1 phenotypes and shrunk tumors.18,19
Taking a slightly different approach, a group at the Karolinska Institute in Sweden recently described success using a drug that targets a surface protein called macrophage receptor with collagenous structure (MARCO), which is preferentially displayed by immunosuppressive M2 TAMs from several types of mouse cancers and human melanoma and breast cancer. The researchers found that in a mouse model of breast cancer, the treatment shifted the balance of macrophages to favor M1s, promoted T cell–dependent immune responses, restricted the size of the animals’ tumors, and reduced the incidence of metastasis.20
It seemed like these macrophages were converting to what could be an anti-tumor phenotype.—Jennifer Guerriero, Dana-Farber Cancer Institute
Yet another strategy involves altering TAM epigenetics. Last year, a team led by researchers at Dana-Farber Cancer Institute in Boston and GlaxoSmithKline in Cambridge, Massachusetts, published findings concerning TMP195, a drug that inhibits histone deacetylases. Testing it in a mouse model of breast cancer, the team found that the treatment caused more macrophages to migrate into tumors, and that most of these cells did not take on an M2 phenotype; instead, they set to work phagocytosing cancer cells.21 Although the role of histone acetylation in macrophage function remains unclear, “it seemed like these macrophages were converting to what could be an antitumor phenotype,” says Dana-Farber immunologist Jennifer Guerriero. Sure enough, treatment with TMP195 alone or in combination with chemotherapy or anti-PD-1 antibodies significantly slowed tumor growth in the animals.
As researchers strive to develop drugs that can shift tumors’ macrophage makeup toward the M1 phenotype, however, they’re learning that the M1/M2 distinction is a bit oversimplified. “M1 and M2 have been used for a long time now and have been a successful way to show how plastic the cells are,” says Pittet. But M1 and M2 are extreme ends of a spectrum. “The in vivo reality is very different. There may be cells that have both phenotypes. There may be some that have neither phenotype but are still very important.”
TAM function may also differ depending on the cells’ location within a tumor or on whether they are derived from circulating monocytes or tissue-resident macrophages. Last year, a group at Washington University School of Medicine in St. Louis reported that TAMs from a mouse model of pancreatic cancer contained both, and that tissue-resident TAMs were more likely to contribute to tissue remodeling to facilitate tumor growth.22 Joyce’s team also recently reported that both bone marrow–derived macrophages and brain-resident microglia contribute to the TAM population within mouse and human brain cancers, but that the two cell types could be distinguished by their gene activation profiles.23 “We know there are multiple different populations of [tumor] macrophages,” she says. “They potentially have quite distinct functions.”
Joyce adds that it’s important to understand how these different TAM subsets influence responses to cancer therapies. For example, she says, it’s possible that some drugs target multiple macrophage types when targeting just one might be better. “That’s the challenge that we have going forward as a field.”
Kaylee Schwertfeger, a pathologist at the University of Minnesota, agrees. “In order to harness their antitumor capabilities, we need to be able to understand the different subtypes in their contexts.”
Amanda B. Keener is a freelance science writer living in Denver, Colorado.
References
- R. Majeti et al., “CD47 is an adverse prognostic factor and therapeutic antibody target on human acute myeloid leukemia stem cells,” Cell, 138:286-99, 2009.
- R.D. Leek et al., “Association of macrophage infiltration with angiogenesis and prognosis in invasive breast carcinoma,” Cancer Res, 56:4625-29, 1996.
- E.Y. Lin et al., “Colony-stimulating factor 1 promotes progression of mammary tumors to malignancy,” J Exp Med, 193:727-40, 2001.
- E.Y. Lin et al., “Macrophages regulate the angiogenic switch in a mouse model of breast cancer,” Cancer Res, 66:11238-46, 2006.
- M. De Palma et al., “Tie2 identifies a hematopoietic lineage of proangiogenic monocytes required for tumor vessel formation and a mesenchymal population of pericyte progenitors,” Cancer Cell, 8:211-26, 2005.
- J.B. Wyckoff et al., “Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors,” Cancer Res, 67:2649-56, 2007.
- A.S. Harney et al., “Real-time imaging reveals local, transient vascular permeability, and tumor cell intravasation stimulated by TIE2hi macrophage-derived VEGFA,” Cancer Discov, 5:932-43, 2015.
- A.S. Harney et al., “The selective Tie2 inhibitor rebastinib blocks recruitment and function of Tie2Hi macrophages in breast cancer and pancreatic neuroendocrine tumors,” Mol Cancer Ther, 16:2486-2501, 2017.
- B.D. Robinson et al., “Tumor microenvironment of metastasis in human breast carcinoma: A potential prognostic marker linked to hematogenous dissemination,” Clin Cancer Res, 15:2433-41, 2009.
- B. Qian et al., “A distinct macrophage population mediates metastatic breast cancer cell extravasation, establishment and growth,” PLOS ONE, 4:e6562, 2009.
- B. Ruffell et al., “Macrophage IL-10 blocks CD8+ T cell-dependent responses to chemotherapy by suppressing IL-12 expression in intratumoral dendritic cells,” Cancer Cell, 26:623-37, 2014.
- O.C. Olson et al., “Tumor-associated macrophages suppress the cytotoxic activity of antimitotic agents,” Cell Rep, 19:101-13, 2017.
- S.P. Arlauckas et al., “In vivo imaging reveals a tumor-associated macrophage–mediated resistance pathway in anti–PD-1 therapy,” Sci Trans Med, 9:eaal3604, 2017.
- 1M.P. Chao et al., “Calreticulin is the dominant pro-phagocytic signal on multiple human cancers and is counterbalanced by CD47,” Sci Transl Med, 2:63ra94, 2010.
- 1S.R. Gordon et al., “PD-1 expression by tumour-associated macrophages inhibits phagocytosis and tumour immunity,” Nature, 545:495-99, 2017.
- 1K. Weiskopf and I.L. Weissman, “Macrophages are critical effectors of antibody therapies for cancer,” MAbs, 7:303-10, 2015.
- K. Weiskopf et al., “Engineered SIRPα variants as immunotherapeutic adjuvants to anticancer antibodies,” Science, 341:88-91, 2013.
- M.M. Kaneda et al., “PI3Kγ is a molecular switch that controls immune suppression,” Nature, 539:437-42, 2016.
- L. Sun et al., “Resveratrol inhibits lung cancer growth by suppressing M2-like polarization of tumor associated macrophages,” Cellular Immunol, 311:86-93, 2017.
- A.-M. Georgoudaki et al., “Reprogramming tumor-associated macrophages by antibody targeting inhibits cancer progression and metastasis,” Cell Rep, 15:2000-11, 2016.
- J.L. Guerriero et al., “Class IIa HDAC inhibition reduces breast tumours and metastases through anti-tumour macrophages,” Nature, 543:428-32, 2017.
- Y. Zhu et al., “Tissue-resident macrophages in pancreatic ductal adenocarcinoma originate from embryonic hematopoiesis and promote tumor progression,” Immunity, 47:323-38, 2017.
- R.L. Bowman et al., “Macrophage ontogeny underlies differences in tumor-specific education in brain malignancies,” Cell Rep, 17:2445-59, 2016.
Interested in reading more?