ABOVE: © iStock.com, Dr_Microbe
Like all of the cells in our body, immune cells age. Over time, they become less and less able to fight infection, cancer, and disease. Previously, researchers thought the process of cells growing old and feeble, known as cellular senescence, was an inevitable consequence of routine infection and time. But a study published yesterday (September 15) in Nature Cell Biology suggests that an interaction between T cells and antigen presenting cells (APCs) early in the immune response to viruses may determine how fast T cells decline.
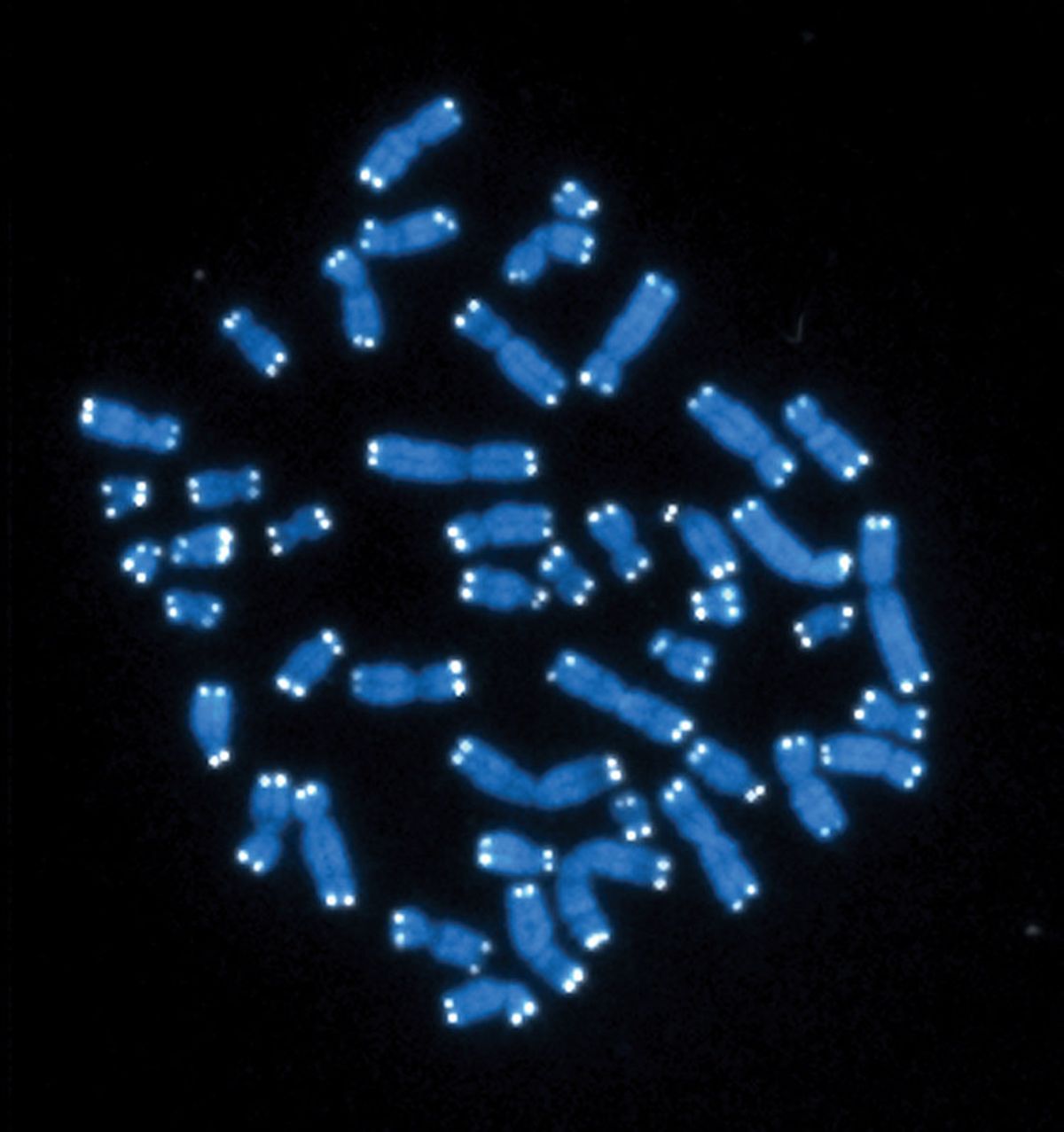
Telomeres are long, repeating sequences of DNA that bookend chromosomes and protect their ends from fraying. As cells age, their telomeres get shorter and shorter with each cell division until eventually, they can no longer divide. The new study finds that after infection, APCs, the cells that initially kickstart T cells’ immune response by presenting them with a foreign antigen, chop off and deliver their telomeres to T cells, the white blood cells that fight viruses.
The researchers found that when APCSs deliver their telomeres to T cells, the latter shift into stem cell-like configuration, which delays their senescence. The researchers also found that this interaction boosts long-term immunity in mice, suggesting that this finding could pave the way for more efficient vaccination.
“This paper is really fascinating,” says Anthony J. Corravubias, an immunologist at UCLA who was not involved in the study. He says that the paper “shed[s] light on a really interesting mechanism that prevents T cells from becoming senescent.”
Cellular life extension via telomeres
When a foreign invader such as a virus enters the body, T cells rapidly divide, and their numbers skyrocket. Previously, scientists knew that T cells employ telomerase, an enzyme that extends telomeres, to combat telomere loss during this rapid division, which over time can lead to shortened telomeres and eventual senescence. But telomerase isn’t sufficient to prevent T cell senescence, sending scientists searching for another key mechanism responsible for guarding against T cell aging.
The researchers, a team at University of College London led by immunologist Alessio Lanna, were initially interested in the role telomeres play in immune cell aging and were analyzing telomere length during the immune response when they uncovered the telomere donation. (Lanna is also the CEO of Sentcell, a biotechnology company that aims to increase human lifespan by rejuvenating T cells.)
To isolate immune cells, Lanna and his collaborators derived T cells and APC cells from the blood of human research participants, then cultured these cells. Then they exposed the cells to a mixture of antigens composed of pieces of various viruses, to ensure that the APC and T cells joined up to replicate a real immune response. Finally, they analyzed the length of the cells’ respective telomeres with a sequencing technique.
See “Can Destroying Senescent Cells Treat Age-Related Disease”
“We were looking at immune synapses between T cells and antigen presenting cells when we made an unexpected observation,” says Lanna. When the APC and T cells they were observing joined up, the T cell telomeres grew longer, while APC telomeres shrank. This action extended the receiving T cells’ telomeres up to 30 times more than telomerase would.
To figure out whether the APCs were indeed donating their telomeres, the researchers labeled APC telomeres with fluorescent markers. After the cells were presented with an antigen, the team of scientists saw clusters of telomeres leaving the APC nuclei and gathering at the junctions between APC cells and T cells. The researchers then isolated these telomere-filled vesicles using fluorescence-activated vesicle sorting. After the APC-derived vesicles were delivered to T cells, even in the absence of APCs, the T cells took up the APC telomeric DNA and tacked it onto the ends of their chromosomes.
These vesicles increased T cell proliferation and decreased the number of T cells with senescence marker proteins, and protected populations of T cells with short telomeres from early aging, the team found. There was also an increase in the number of stem-like memory T cells, which are able to perform either effector or memory functions if they encounter a pathogen again. Effector cells are involved in increasing inflammation and killing infected cells, while memory cells hold on to information about threats to the body to kickstart future immune responses.
Previous studies from other groups had determined that in the more stem cell–like configuration, T cells live longer than those that have differentiated, says Lanna. The results suggest that the fate of some T cells—whether they become senescent or not—is determined when APCs deliver telomeres to T cells. This means that some T cells’ destinies are sealed before the immune response has even started. “That’s against dogma in the field of immune senescence,” says Lanna.
In vivo immunity boost
This telomere donation also appears to boost immunity long term in mice. In another experiment, the researchers exposed T cells to a flu vaccine, then exposed one group of T cells to APC-derived telomere-filled vesicles, and another group to vesicles without telomeres. They then injected T cells into separate groups of mice that were also exposed to H1N1, a strain of influenza commonly referred to as swine flu. Mice that didn’t receive any sort of treatment died almost instantly from the flu, but both types of T cell treatment seemed to protect the mice after the virus injection. After 15 days, the researchers exposed both groups of mice to H1N1 again. The mice that had received the T cells exposed to telomere-filled vesicles still had a robust immune response to the H1N1 injection, but the other T cell–treated group died immediately. This suggests that APC-derived vesicles might help T cells maintain their immune function over time, the researchers say.
“We know we can administer these vesicles to an animal and that will protect the animal in the long term from infection,” says Lanna. The vesicles could even be incorporated into vaccines to extend the effectiveness of immunization, he suggests, or eliminate the need for boosters.
The researchers also observed that APCs deliver telomeres to some T cells and not others, although it’s not clear why. Using Flow-FISH, an assay that counts cells and analyzes their telomere length one by one, the team found that naive T cells—cells that have never encountered an antigen—and memory T cells were more likely to take up telomeres. Meanwhile, various types of effector T cells are less likely to do so.
In addition to their potential application to vaccines, these discoveries may open up the possibility of treatments that stimulate APC vesicle release and make T cells more likely to accept vesicles, or technologies that extract and deliver vesicles, Lanna says. T cell senescence has been linked to increased risk of infections, cancers, and dementia, he adds, and such treatments could potentially help delay immune aging and associated diseases.
“I think it’s a really awesome study that has a lot of potential in the clinic, as far as making vaccines more efficient,” says Corravubias. In addition, “it’d be interesting if you could treat patients that are either undergoing a chronic infection, or as a preventative way to help them boost their immunity towards different infections.”





